I have had a day that was not so wonderful this week, but apart from that the placement has been going well. Last week, interspersed with the stroke-related dietetics, we had a day with the dietitians at a medium-secure mental health hospital.
It was an incredible experience. The workload of the dietitians there is fairly ordinary - the usual heart disease, obesity, high cholesterol, type 2 diabetes, hypertension and other conditions that you'd find in any population, but the secure setting makes the job quite different and extraordinary. Doors are locked, dietitians are never left alone with patients, and everything is risk-assessed - patients are there because they have exhibited behaviour that presents a danger to themselves and/or to others. The ethical issues are in your face: people are locked up, but must still consent to the treatment that is offered (as long as they are deemed to have capacity to do so).
The thing that had the greatest impact on me is that all these patients have to be contained in the same place, so there is very little 'normality' in evidence, to remind patients what 'normal' is - not even a paperclip can be left on a ward, let alone the option to go out for a pint, watch what you want on TV, use the Internet or a mobile phone. In my everyday life, I never see the kind of disturbing scenes that are routine in one of these units. You're having to live in close proximity to all of this, have virtually all your autonomy removed from you, while you are recovering from your own serious illness. It must be very difficult. The adolescent unit was particularly uncomfortable to observe.
At the weekend there were a surprising number of potential dietetic interventions: lunch with type 2 diabetes and dementia, tea with coeliac disease, more tea with colon cancer, and a movie with alcohol-related concussion.
Mr A's father has diabetes that he manages to control solely with his diet, and he is fit and well and over 80 now. Mr A's mother, unfortunately, has a form of dementia that is making slow but inexorable progress, and she was pretty bad at the weekend. She has developed very fixed ideas, some of which are imaginary or delusional, and she can become very confused. We took The Boy down with us to visit them for lunch.
One of Mr A's mother's fixed ideas is that I am wonderful, so she clamps onto me like a limpet and talks to me incessantly. She was born in Wales, Mr Beeching is terrible for shutting all the railway stations, so was Mrs Thatcher, Mr A was born during the Falklands war (he would have to be about 30 years younger for that to be true), the Germans are awful because of what they did in the war, the Scots are taking over the government (she thinks David Cameron is Scottish because of his name), her mother slept with American GIs during the war, she has inherited a THOUSAND pounds. The Germans are awful because of what they did in the war, so is Mr Beeching and Mrs Thatcher, so are the Scots, and her mother too. She was born in Wales. And so it goes on, round and round.
After lunch we went on to visit a family who used to look after The Boy when he was a child, and discovered that his 'surrogate grandmother' was diagnosed with coeliac disease some years ago. She is one of the jolliest, smiliest ladies I've ever met. The final visit of the weekend was to some friends, one of whom had recently been treated for colon cancer, and is waiting to find out if further treatment is needed. And The Boy himself had recently did some damage to himself by tripping up and planting his face into the ground, losing half a front tooth and giving himself concussion. But he's fine now.
Thursday 29 July 2010
Sunday 25 July 2010
Stroke week
Week 5 of my 12-week placement was supposed to be Stroke Week with an emphasis on Peer-Assisted Learning. Except it didn't work out entirely as planned, for two reasons: my peer was off sick on Monday, and on Wednesday we didn't do anything about stroke. The other issue was that all of the dietitians qualified to work on the wards were away on Thursday and Friday except for the one who was supposed to supervise us students, making her job a completely impossible one.
On Monday, then, instead of working with my peer I went off to some other (non-stroke) wards to see new patients. I have started, very carefully, to be allowed to talk to the patient and ward staff. It is more difficult than it sounds, believe me, and almost harder than writing in the dietetic and clinical records.
I so much prefer the controlled atmosphere of an outpatient or community consultation, where the absolute maximum amount of distraction might be from one or two family members. There is so much going on in the wards, I can hardly think straight. Part of the difficulty lies in continually switching between wards and patients so that there is no continuity or familiarity - when I am ultimately given more responsibility, I should be able to get a bit of routine into the work, which should make it all easier and less stressful.
Alongside the practical experience there are some 'tutorials' which take the form of worksheets covering the specialist area of the week. In the stroke tutorial, apart from revising some aspects of stroke incidence and care, we had to invent a 'feed regimen' for someone who initially needed to be fed through a tube, and then moved on to start eating again. It was a lot harder than it looked, but we both came up with something that wasn't too bad.
Because of the structure of the training this week, and the shortage of staff, J and I have spent a lot of the week together on the stroke ward. We observed some of the work that the physiotherapists do to help people become more mobile following a stroke, at breakfast time and in the 'gym'. We watched a couple of swallowing assessments with a Speech and Language Therapist (SALT), which was fascinating. SALTs seem to have two quite distinct areas of specialism, communication and swallowing, but they are clearly related by the requirement for coordination of brain impulses, tongue and oesophageal muscle control.
On Thursday and Friday we started this Peer-Assisted Learning thing in earnest. It involved going through a dietetic record card and clinical records for both new and existing patients, then writing our hypothetical entries in the records. We didn't do too badly, but it brought home how much we still have to learn. Quite a lot of the proposed treatment plan has to be based on experience, which we obviously don't have yet. It's getting better with practice, though.
On Monday, then, instead of working with my peer I went off to some other (non-stroke) wards to see new patients. I have started, very carefully, to be allowed to talk to the patient and ward staff. It is more difficult than it sounds, believe me, and almost harder than writing in the dietetic and clinical records.
I so much prefer the controlled atmosphere of an outpatient or community consultation, where the absolute maximum amount of distraction might be from one or two family members. There is so much going on in the wards, I can hardly think straight. Part of the difficulty lies in continually switching between wards and patients so that there is no continuity or familiarity - when I am ultimately given more responsibility, I should be able to get a bit of routine into the work, which should make it all easier and less stressful.
Alongside the practical experience there are some 'tutorials' which take the form of worksheets covering the specialist area of the week. In the stroke tutorial, apart from revising some aspects of stroke incidence and care, we had to invent a 'feed regimen' for someone who initially needed to be fed through a tube, and then moved on to start eating again. It was a lot harder than it looked, but we both came up with something that wasn't too bad.
Because of the structure of the training this week, and the shortage of staff, J and I have spent a lot of the week together on the stroke ward. We observed some of the work that the physiotherapists do to help people become more mobile following a stroke, at breakfast time and in the 'gym'. We watched a couple of swallowing assessments with a Speech and Language Therapist (SALT), which was fascinating. SALTs seem to have two quite distinct areas of specialism, communication and swallowing, but they are clearly related by the requirement for coordination of brain impulses, tongue and oesophageal muscle control.
On Thursday and Friday we started this Peer-Assisted Learning thing in earnest. It involved going through a dietetic record card and clinical records for both new and existing patients, then writing our hypothetical entries in the records. We didn't do too badly, but it brought home how much we still have to learn. Quite a lot of the proposed treatment plan has to be based on experience, which we obviously don't have yet. It's getting better with practice, though.
Wednesday 21 July 2010
Shiny red toes

Outside work there's been a little bit of activity, which on top of the week's work has exhausted me. I'm definitely not as young as I was.
On Friday we journeyed south to the Ealing Comedy Festival, to see Henning Wehn in particular and a bunch of other comedians in general. Unfortunately, Henning Wehn was one of the best acts on the bill, and he was only given about 10 minutes at the beginning of the show. One of the comedians was so poor that I felt no shame in leaving the tent to go to the toilet during his act - luckily, I was near the end of the row of seats. We also had some painfully noisy punters behind us, yelling incomprehensibly and deafeningly loudly. It wasn't anything like as good as I'd hoped, unlike the pre-show cocktail provided by Mr M, which was very fine indeed.
Saturday was Family Day. Lola II treated me to a pedicure, which I've never had before. I liked the bit where you put your feet into warm water, and the bit where the pedicurist massages oil into your feet, and the lovely shiny new red toes. I didn't like the cuticle-trimming bit, nor the bit where she buffed my nails before putting on the polish. Combined with the need to check every preparation for parabens and tocopherol (both of which bring me out in a rash), it was less luxurious and relaxing than I'd hoped.
So it was also a bit disappointing, but the lovely pedicure lady and Lola II and mum arriving to chat halfway through were some compensation. I was also able to give mum a present I'd been saving for her for a while - a biro with the ink nearly run out. She loves to finish off a biro and throw it away, so I always try to save mine for her when they get to that state.
We were scheduled for Good Deeds for the rest of Saturday morning at Lola II's house. Dad fitted fancy covers on the screws holding Lola II's bathroom mirror. Mr A was supposed to help dad with his computer, but failed to find the correct port to plug in the screen until brother-in-law (BiL) arrived. BiL swiftly started on the installation of a security light, Mr A worked on the software installation using his laptop for backup, while Lola II and I tried to schedule train tickets to Altrincham using a laptop each and cross-checking. Then the delivery van turned up with Lola II's bed which they constructed in her bedroom, Mr M and Mr A moved a dresser upstairs and a piano downstairs (!), we ordered Persian food for lunch from a takeaway menu, Mr M went to pick it up and sister D arrived. We had lunch (delicious), transferred a microwave from one car to another, loaded dad's computer back into his car, and set off home.
I had to let Mr A take over the driving when we were only halfway home, and I went to sleep for two hours when we arrived.
There is one other irrelevant yet vaguely interesting event to report. The way that our TV reports our viewing to the BARB panel was malfunctioning, so they got in touch and asked if we'd mind if they sent an engineer round to try and fix it. I am keen to accommodate them in every way, because they will soon be financing a new dishwasher in the same way as they contributed to my ipod.
Some time ago we acquired a Sky box, in the knowledge that when Digital Switchover comes to our area we'd need something to receive it. Our house came with a satellite dish that we never bothered to remove, so we plugged everything in. It seemed to work for a day or two, and then stopped, and we did nothing at all about it because we're really not very interested in most TV. When the BARB engineer came round he moved the card from one slot to another slot indistinguishable in every way from the first slot, and then when I came home from badminton Mr A was watching The Last Samurai on ITV2.
Last time we had temporary access to tens of channels instead of just four, we watched a couple of old episodes of The Sweeney and Starsky and Hutch and then went straight back to BBCs 1 and 2 like the middle class Radio 4 listeners that we are. I expect the same will happen this time.
Sunday 18 July 2010
Renal week
This Dietetics department contains lovely people. Of course, there are things that might be improved, but on the whole, it works very well, and I am having a high quality experience on this placement. Last week was renal week, and unlike paediatric week, I've actually been almost exclusively working in renal situations.
I attended a 'Ward Round' which was remarkably similar to the one depicted in 'Doctor in the House' more than 50 years ago, with Sir Lancelot Spratt played by James Robertson Justice and Dirk Bogarde as Simon Sparrow. Except the doctor was probably in her 30's, female, and black, and she actually spoke to the patients. I thought she did a pretty good job at juggling the fairly obscure clinical jargon and the need to ensure that the patients understood what was going on. They were even offered choices, although I'm not sure what would have happened if they hadn't agreed with the option that was proposed for them.
A Dietitian on the acute hospital renal ward has fairly low status, and this is probably realistic - dialysis and controlling infection is definitely more important than a low potassium diet for these patients. Just getting them to eat enough is a challenge, because when there's something wrong with your kidneys it seems you generally feel pretty rubbish and not particularly interested in food.
I was looking forward to the outpatient clinic, where patients really rely on good dietary advice in order to avoid complications and put off the need for dialysis as long as possible. Unfortunately, outpatients were thin on the ground for some reason, and we only saw two in a morning, one needing advice on restricting potassium and the other on restricting phosphate. Obviously we were guaranteed to see patients at the Dialysis Centre, where I was able to practise my diet history taking technique, and then back on the ward for another Ward Round on Friday. Different doctor in charge, but same attention to communicating with the patients.
Renal week overall lesson for the future: if you like cheese, chocolate and tomatoes as much as I do, then try to look after your kidneys. This means keeping your blood pressure under control, and make sure you manage your blood sugar properly too if you have diabetes.
In between long days trying to hone my skills at writing concise dietetic notes in records, J and I went out after work for a pizza with some of the team. When the time came to split the bill, there was a little bit of cash left over - most of it went towards the department tea and coffee kitty, but they made J and me take a £1 refund. This was most thoughtful - after all, we're not being paid for our labours. J has been having a hard time with her shared accommodation as well, so an evening out in such good company was quite lovely.
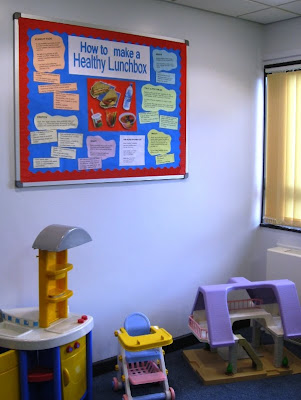
 Thankfully the office has been cooler since the weather broke this week, although it's still hot enough to wear sleeveless vests. J and I finished our Healthy Lunchbox noticeboard, and it's now displayed in all its glory in the Children's Waiting Area. Click on the small image if you want a version that you can enlarge and read.
Thankfully the office has been cooler since the weather broke this week, although it's still hot enough to wear sleeveless vests. J and I finished our Healthy Lunchbox noticeboard, and it's now displayed in all its glory in the Children's Waiting Area. Click on the small image if you want a version that you can enlarge and read.Wednesday 14 July 2010
Week three
I want to write, I really do. I want to sit down quietly at the end of a long and fascinating day, and spend some time thinking, reflecting, pondering on the events of the day. What that patient was thinking, there in that bed, with all their relatives sitting around. How they had reached this point in their life, in a hospital, needing so much help. What the ward staff are doing, whizzing about without a minute to sit with someone and reassure them. How many people rush about the whole time, looking after a ward full of sick people. How much noise and bustle there is, so much efficiency, and yet often so ineffective, care full of holes.
But at the end of a day I drive home, Mr A and I muster something to eat, and I'm tired. Writing is a solitary activity, and I like to talk to him, spend time with him rather than in my room at the computer. Even if we're just watching a DVD together, it's together rather than individually. Although being asked to help with integrating equations involving sines and cosines at 7 a.m. took being together a little too far last week, even for me. Mr A is finding the maths modules considerably more challenging than the computing ones.
There's really a lot going on at 'work'. Most days I shadow one or other of the dietitians in their daily clinics, either in the Dietetic department (in a separate building on the hospital site) or on the wards. Last week, in addition to paediatrics, I spent time on an orthopaedic ward, a renal ward, the ITU (Intensive Therapy Unit) and a general outpatient clinic.
In the general clinic I can just about imagine running a consultation, but the wards are still too much for me, especially ITU. Each ward is organised differently, the notes are kept in three different places, and even though there's usually a white board listing the patients' names, they are sometimes organised by location on the ward, sometimes by surname, and sometimes by the supervising consultant. Often there is information missing: fluid or food intake, bowel movements, whether food or drink given was actually eaten or drunk. There is often no accurate weight, which is the main criterion we can use (alongside dietary components in blood measurements) to determine whether a dietary therapy is working or not.
J and I also spent a morning being shown around the Pharmacy department - there are more than 100 members of staff working there, one third qualified Pharmacists, one third Technicians (not quite so qualified) and the rest unqualified or administrative staff. As well as managing purchasing and distribution of drugs around the hospital, they also make up the preparations used in cancer treatment in aseptic rooms, and would also make up bags for intravenous (parenteral) nutrition if this wasn't contracted out at the moment. There's a Medicines Information section whom you call if you have any queries about pharmaceuticals - for example, if someone were being fed exclusively through a tube, how a tablet designed for swallowing might be administered.
J and I have also been collaborating on our healthy lunchbox task. We've decided what the display might include, and spent a happy half-day printing pictures and text, cutting them out and mounting on card and then sticking them onto a large sheet of paper to see how they looked. Our supervisor made some useful comments, and this week we are constructing the final version.
But at the end of a day I drive home, Mr A and I muster something to eat, and I'm tired. Writing is a solitary activity, and I like to talk to him, spend time with him rather than in my room at the computer. Even if we're just watching a DVD together, it's together rather than individually. Although being asked to help with integrating equations involving sines and cosines at 7 a.m. took being together a little too far last week, even for me. Mr A is finding the maths modules considerably more challenging than the computing ones.
There's really a lot going on at 'work'. Most days I shadow one or other of the dietitians in their daily clinics, either in the Dietetic department (in a separate building on the hospital site) or on the wards. Last week, in addition to paediatrics, I spent time on an orthopaedic ward, a renal ward, the ITU (Intensive Therapy Unit) and a general outpatient clinic.
In the general clinic I can just about imagine running a consultation, but the wards are still too much for me, especially ITU. Each ward is organised differently, the notes are kept in three different places, and even though there's usually a white board listing the patients' names, they are sometimes organised by location on the ward, sometimes by surname, and sometimes by the supervising consultant. Often there is information missing: fluid or food intake, bowel movements, whether food or drink given was actually eaten or drunk. There is often no accurate weight, which is the main criterion we can use (alongside dietary components in blood measurements) to determine whether a dietary therapy is working or not.
J and I also spent a morning being shown around the Pharmacy department - there are more than 100 members of staff working there, one third qualified Pharmacists, one third Technicians (not quite so qualified) and the rest unqualified or administrative staff. As well as managing purchasing and distribution of drugs around the hospital, they also make up the preparations used in cancer treatment in aseptic rooms, and would also make up bags for intravenous (parenteral) nutrition if this wasn't contracted out at the moment. There's a Medicines Information section whom you call if you have any queries about pharmaceuticals - for example, if someone were being fed exclusively through a tube, how a tablet designed for swallowing might be administered.
J and I have also been collaborating on our healthy lunchbox task. We've decided what the display might include, and spent a happy half-day printing pictures and text, cutting them out and mounting on card and then sticking them onto a large sheet of paper to see how they looked. Our supervisor made some useful comments, and this week we are constructing the final version.
Sunday 11 July 2010
What I've been reading
Imperium
by Robert Harris
"Ancient Rome teems with ambitions and ruthless men, none more brilliant than Marcus Cicero. A rising young lawyer, backed by a shrewd wife, he decides to gamble everything on one of the most dramatic courtroom battles of all time. Win it, and he could win control of Rome itself. Lose it, and he is finished forever."Aah, reading for pleasure again. Nothing better than sitting on holiday with the rain pattering on the conservatory glass roof and reading a nice, light (but historically believable) thriller novel.
Vile Bodies
by Evelyn Waugh
narrated by Robert Hardy
"The Bright Young Things of 1920s Mayfair, with their paradoxical mix of innocence and sophistication, exercise their inventive minds and vile bodies in every kind of capricious escapade, whether it is promiscuity, dancing, cocktail parties, or sports cars. A vivid assortment of characters hunt fast and furiously for ever greater sensations and the hedonistic fulfilment of their desires."I needed more Evelyn Waugh after admiring the lyrical narration of Brideshead Revisited, and this book reminded me of the wonderful black humour of his writing, which was absent from Brideshead. This isn't the best of his work, but I enjoyed it a lot. Much more audio book action to come, now that I'm commuting again.
An Infamous Army
by Georgette Heyer
narrated by Claire Higgins
"'Why, Charles, whom can you be staring at?' she began, but broke off as her gaze followed his. It was quite obvious whom Colonel Audley was staring at. He was staring at a vision in palest green satin draped in a cloud of silver net. The Lady Barbara Childe had arrived, and was standing directly beneath a huge chandelier, just inside the ballroom."Now, I like reading Georgette Heyer, and I'm sure she included a great deal of historical accuracy in this account of a love affair set in the background of the Battle of Waterloo. I learned that the battle didn't really take place at Waterloo, but that was the village in which the Duke of Wellington stayed the previous night, and I have picked up the names of many of the distinguished commanders of various divisions of infantry and cavalry. But that's not why I read Ms Heyer, and there really was too much swashbuckling and not enough handsome swain. The last three hours of the book were an account of the battle, with about 20 minutes at the end for the two lovers to become reconciled.
Friday 9 July 2010
Paediatric dietetics

This week the focus was on paediatric dietetics. This is a fairly complex area, and is introduced at the start of the placement when we're still finding our feet because there isn't a whole lot we can do to contribute - later in the placement we need more straightforward cases to practise on.
I observed three paediatric outpatient clinics in the Dietetic department, which included children with cow's milk intolerance, coeliac disease, low weight for their age (now called 'faltering growth' rather than 'failure to thrive'), and high weight for their age (now called 'obese' rather than 'bonny' or 'chunky'). There were some children who have difficulty eating more than a very narrow range of food. Some parents were obviously well-informed about the need for dairy foods, fruit and vegetables. Some were not.
One interesting session was a 'feeding group' where the dietitian is joined by a speech & language therapist and a psychologist, to address particularly difficult issues that may have psychological, behavioural or clinical causes. I learned a lot about children, formula milk, calcium-containing non-dairy foods, parents, feeding and mealtimes. Fact: rice milk is not suitable for feeding to dairy-intolerant children under the age of five, because of the risk of arsenic contamination. Choose calcium-fortified oat milk or soya milk instead. No, I have no idea what they taste like, either.
It's not an area that particularly excites me, particularly as I find myself becoming quite tense about the behaviour of some of the children (and some of the parents), without the moderating effect of having had children of my own to compare with. Not all parents of naughty children are bad parents. Sometimes children are naughty in spite of their upbringing. All I know is that it must be particularly difficult to cope if one of your children isn't allowed to eat what the others do. Or won't eat anything except dry toast. Or vomits persistently and won't eat solids even though s/he is two years old.
I did get some practical, hands-on experience though, even if it was just weighing children and measuring their height. A particular highlight this week was my first 'Diet History', where I took down the salient features of a typical day's intake from a very articulate 8 year-old child with coeliac disease. This is actually more significant than it sounds, because it forms part of the assessment of my competence. In just eight weeks time, I should be proficient not just in taking diet histories, but in conducting the whole consultation, although with adults rather than 8 year-olds. It seems less unachievable now that I've actually taken the first step.
Saturday 3 July 2010
Screening for malnutrition

I know, it's been ages. Working 9 to 5 with an hour's commute each way removes a lot of the time I used to employ for blogging, and there's nothing I can do about it. Evenings are precious time now.
The good news is that the placement is going very well, and incomparably better than my A placement two years ago, thank goodness. The department's staff are extremely supportive and generally nice to be with, and we two students are being given just the right amount of work to do - not so much that we are daunted but enough to keep us occupied, despite having few of the skills required to do anything very useful. It's still very hot indeed in the office, which makes it quite an effort to concentrate towards the end of a long day.
I've mentioned before that many people are malnourished on admission to hospital, and one of the ways to deal with this is to enable many healthcare workers to make an objective assessment of the level of malnutrition. I attended a nutrition screening training session led by the hospital's Nutrition Sister (a senior nurse responsible for nutritional matters). Only two out of the seven potential attendees actually turned up, plus me and a student nurse. The training was intended to cover the importance of food and nutrition in the hospital setting, the different ways that food can be delivered to patients, and how to use a scoring tool to measure the level of malnutrition.
Many places use a tool known as MUST - Malnutrition Universal Screening Tool - which scores on just three criteria: current BMI, degree of recent weight loss, and low oral intake or risk of reduced intake into the future. MUST is often used in community settings like nursing and residential care homes, but within this hospital there is a different scoring system, with about ten assessment measures producing a score that can trigger a referral to a Dietitian if it reaches 15 or above.
That was last week. This week my fellow student J and I attended a training session delivered by a senior dietitian on nutritional screening and identifying and dealing with risk of malnutrition, but intended for staff of nursing homes: nurses, care workers and catering staff. Again, only two of the eight attendees who had signed up for the half day actually turned up. It's possibly an indication of the pressure that staff are under, since last minute difficulties at work probably prevented them from attending, rather than lack of interest, but who knows? Perhaps they just couldn't be bothered.
I have been introduced to some more of the administrative requirements of the dietitian's job, including the medical notes, and spent quite a lot of time shadowing dietitians on their visits to patients on the hospital wards. We have also been given a few projects to do, including three talks between the two of us. My individual one is to residents of sheltered housing, and I'm doing one together with J to staff supporting adults with learning disabilities living in the community. Both will be about healthy eating in general.
J and I also have a Health Promotion assignment to do together, which is a display for a noticeboard in the Children's Waiting Area. We are hoping to do something about lunchboxes. We've also collaborated on entering a mountain of menus into the nutritional analysis software used in the department, which is a whole lot easier than the one used in the university, but still pretty tedious.
The last thing I did on Friday, and the focus of the coming week, is paediatric dietetics. But you'll have to wait to hear about that.
Subscribe to:
Posts (Atom)